Transform Your Diagnostic Practices: Harness the Latest Innovations in Blood Testing
Achieve Exceptional Diagnostic Accuracy with High-Sensitivity Assays
The emergence of high-sensitivity assays represents a revolutionary step forward in the field of diagnostics, specifically designed to significantly enhance the accuracy of medical evaluations. These advanced assays are meticulously crafted to identify even the most minute concentrations of biomarkers present in blood samples, a pivotal element for the early detection of a wide range of diseases. For instance, in the realm of oncology, the ability to detect circulating tumour DNA at extremely low levels enables timely medical interventions, which can greatly improve patient outcomes. The integration of high-sensitivity assays is particularly crucial for rapid diagnostics in critical situations, such as cardiac events or during outbreaks of infectious diseases, where every moment counts.
These innovative assays utilize cutting-edge technologies, including electrochemiluminescence and fluorescence, which amplify signals from biomarkers, making them detectable even in trace amounts. Recent studies indicate that these sophisticated assays can substantially reduce diagnosis time, empowering healthcare providers to initiate treatment protocols without delay. Additionally, the superior specificity and sensitivity of these tests significantly decrease the chances of false negatives, which is particularly critical in scenarios where any delay in treatment could result in severe consequences for patients.
As the healthcare industry pivots towards personalised medicine, the role of high-sensitivity assays becomes increasingly vital for monitoring disease progression and assessing responses to therapeutic interventions. By gaining a deeper understanding of biomarkers and their implications across various health conditions, clinicians can effectively customize treatment plans. This approach not only enhances patient care but also optimizes resource allocation within healthcare systems, fostering improved efficiency and effectiveness in service provision.
Enhance Diagnostic Efficiency and Precision with Automated Blood Testing Technologies
The incorporation of automated systems within blood testing laboratories is fundamentally reshaping diagnostic methodologies, leading to significant improvements in both accuracy and efficiency. By reducing human error, these advanced systems lower the risk of inaccuracies, thereby enhancing blood test accuracy improvements. Automated platforms are capable of processing a vast number of samples far more quickly than traditional manual methods, which is essential for laboratories aiming to keep pace with the growing demand for testing.
Moreover, automation ensures consistency in results across different laboratories by standardizing testing protocols and methodologies. This standardization is particularly crucial in multi-centre studies, where discrepancies can result in conflicting interpretations of results. The latest advancements in robotics and artificial intelligence (AI) are driving the next generation of automated systems, which can conduct tests and analyze outcomes with unparalleled precision. These sophisticated systems employ algorithms that adapt and improve their performance based on historical data, further enhancing reliability.
Additionally, automated systems enable real-time monitoring of test results, providing clinicians with immediate access to vital information. This immediacy is critical in emergency situations, where timely decision-making can be life-saving. As automation technologies continue to evolve, the opportunities for blood test accuracy improvements will expand, making diagnostic processes more rapid, reliable, and ultimately more beneficial for patient care.
Microfluidics: Pioneering Advanced Blood Testing Technologies
Microfluidic technology marks a significant advancement in diagnostics, particularly in enhancing blood test accuracy improvements. By manipulating tiny volumes of fluids at the microscale, these innovative devices offer unparalleled precision in sample handling and analysis. This level of accuracy is especially vital when dealing with limited sample sizes, such as in paediatric or geriatric populations, where every drop counts.
The application of microfluidics in blood testing allows for the simultaneous examination of multiple biomarkers within a single assay, greatly amplifying diagnostic capabilities. For example, a microfluidic chip can be engineered to simultaneously detect various pathogens in a blood sample, providing comprehensive insights into a patient’s health status within minutes. This rapid response time is invaluable in clinical environments, particularly when addressing infectious diseases, where prompt intervention is essential for effective management.
Furthermore, integrating microfluidic devices with advanced imaging techniques can further enhance blood test accuracy. Real-time imaging enables detailed observation of reactions and interactions within samples, leading to more reliable interpretations. As research continues to advance microfluidic technology, its role in bolstering blood test accuracy improvements is set to grow, paving the way for groundbreaking diagnostic solutions that can transform patient care.
Enhancing Diagnostic Capabilities with Advanced Imaging Techniques in Blood Testing
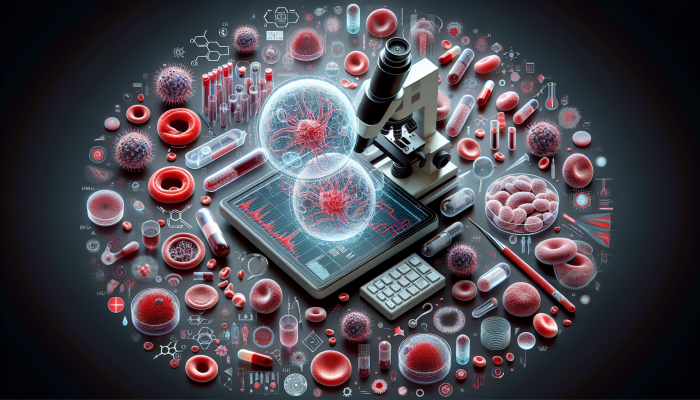
The incorporation of advanced imaging techniques signifies a substantial evolution in blood testing, delivering unprecedented resolution and real-time insights. Techniques such as high-resolution microscopy and digital pathology play a vital role in enhancing blood test accuracy. These methodologies facilitate a more detailed examination of blood samples, allowing for the detection of subtle anomalies that standard testing methods may overlook.
For instance, high-resolution imaging can unveil cellular changes at the microscopic level, which is crucial for diagnosing conditions like leukaemia and other blood disorders. These advanced techniques empower clinicians to visualize and assess the morphology of blood cells with heightened accuracy, leading to more dependable diagnostic results. The capacity to evaluate cellular structures in real-time also enables healthcare providers to make quicker, more informed decisions regarding patient management strategies.
Moreover, combining imaging techniques with machine learning algorithms further enriches the diagnostic process. By training algorithms on extensive imaging datasets, these systems can identify patterns and anomalies that may escape human observation. This synergy not only enhances blood test accuracy but also reduces the time required for analysis, ultimately facilitating faster clinical decision-making. As advancements in imaging technologies continue, their contribution to blood test accuracy improvements will prove invaluable.
Revolutionizing Blood Testing with Breakthroughs in Nanotechnology
The utilization of nanotechnology in blood testing is transforming the diagnostic landscape by providing unparalleled sensitivity and specificity. At the nanoscale, materials exhibit unique properties that can be exploited to create state-of-the-art diagnostic tools. These advancements hold the potential to markedly enhance blood test accuracy improvements, especially in the detection of biomarkers associated with various diseases.
For example, nanoparticles can be engineered to selectively bind to specific biomarkers in the bloodstream, facilitating targeted delivery of diagnostic agents. This precision targeting improves test sensitivity and reduces the incidence of false positives. In conditions like cancer, where early detection is crucial, nanotechnology can aid in identifying tumour markers at concentrations significantly lower than traditional methods can achieve.
Furthermore, the role of nanotechnology extends beyond detection; it is vital in developing advanced drug delivery systems. By designing nanoscale carriers capable of delivering therapeutic agents directly to affected areas, clinicians can enhance treatment efficacy while minimizing adverse effects. This dual functionality of detection and treatment highlights the transformative impact of nanotechnology within the medical field.
As research in nanotechnology progresses, its influence on improving blood test accuracy will become increasingly evident. The ability to detect diseases earlier and with greater precision can lead to enhanced patient outcomes and a more effective healthcare system overall.
Global Initiatives Aiming to Standardize Enhancements in Blood Test Accuracy
Establishing Consistency with Standardized Reference Materials

The implementation of standardized reference materials is a foundational principle in laboratory practices, ensuring uniformity and comparability in blood testing worldwide. These reference materials act as benchmarks for evaluating test results, assisting in the calibration of assays and the validation of testing methodologies. In the pursuit of improving blood test accuracy, the use of reference materials is critical for maintaining the integrity and reliability of test outcomes.
Standardized reference materials are particularly crucial in multi-centre studies, where laboratory results must be compared against one another. By employing identical reference materials, laboratories can ensure accurate and comparable results. This consistency is vital for clinical trials and research studies, where variability in results can lead to erroneous conclusions that jeopardize patient safety.
Furthermore, the development and dissemination of international reference materials by organizations such as the World Health Organization (WHO) bolster global standardization efforts. These materials undergo rigorous testing and validation, providing laboratories worldwide with a reliable means of ensuring the accuracy of their blood tests. As more laboratories adopt standardized reference materials, the overall quality of blood testing will improve, reinforcing confidence in diagnostic practices.
Additionally, the continuous refinement of reference materials is essential to keep pace with advancements in testing technologies. As new biomarkers are discovered and innovative assays developed, the need for updated reference materials becomes paramount. This ongoing commitment to standardization is vital for enhancing blood test accuracy.
Enhancing Reliability through Harmonized Testing Protocols
Standardizing testing protocols across various laboratories represents a crucial initiative aimed at minimizing variability and elevating the reliability of blood test results. Variations in methodologies, reagents, and equipment can lead to substantial discrepancies in test outcomes, undermining the credibility of diagnostic practices. By focusing on harmonizing protocols, laboratories can achieve greater consistency and accuracy in their blood testing processes.
Protocol harmonization is particularly important in large-scale epidemiological studies, where data integration from multiple sources is imperative. When laboratories adhere to standardized protocols, researchers can have confidence that their results are comparable, leading to more robust conclusions and informed public health decisions. This consistency is vital for both research and clinical practice, where accurate test results are essential for effective patient management.
Organizations such as the Clinical and Laboratory Standards Institute (CLSI) play a key role in developing and disseminating standardized guidelines for laboratory testing. By providing clear, evidence-based protocols, these organizations help ensure that laboratories operate within a framework that prioritizes accuracy and reliability. As more laboratories adopt harmonized protocols, the quality of blood test accuracy will continue to improve.
Moreover, the globalization of healthcare necessitates a commitment to protocol harmonization. As healthcare providers increasingly collaborate across borders, the demand for consistent testing practices becomes more pronounced. Harmonization not only enhances the credibility of test results but also promotes greater collaboration and data sharing among laboratories, ultimately benefiting patient care on a global scale.
Implementing Comprehensive Quality Control Measures for Consistent Outcomes
Establishing rigorous quality control measures is crucial for maintaining high standards of accuracy and precision in blood testing. Quality control encompasses a wide range of practices aimed at monitoring and enhancing testing processes, ensuring that laboratories deliver reliable and consistent results. Robust quality control measures are indispensable for driving blood test accuracy improvements.
A core component of quality control involves the regular assessment of laboratory equipment and procedures. This includes routine calibration of analytical instruments, comprehensive training for laboratory personnel, and strict adherence to established protocols. By ensuring that all aspects of the testing process comply with rigorous quality standards, laboratories can significantly reduce the likelihood of errors and inaccuracies in test results.
Additionally, participation in proficiency testing programs allows laboratories to benchmark their performance against their peers. These initiatives provide laboratories with opportunities to evaluate their testing capabilities and identify areas for improvement. By addressing any discrepancies, laboratories can enhance their performance and contribute to the overall advancement of blood test accuracy.
Furthermore, embedding quality control measures into laboratory workflows fosters a culture of continuous improvement. By routinely reviewing and refining testing processes, laboratories can adapt to emerging challenges and maintain high levels of accuracy. This commitment to quality is essential in an era where the demand for reliable blood tests is greater than ever, ensuring patients receive optimal care based on trustworthy diagnostic information.
The unrelenting pursuit of quality control in blood testing is not merely a regulatory requirement; it is a moral obligation to safeguard patient health. As laboratories prioritize quality control measures, the positive impact on blood test accuracy improvements will resonate throughout the healthcare system.
Ensuring Compliance with Regulations for Enhanced Diagnostic Integrity
Adhering to international standards and regulations is vital for enhancing the credibility and acceptance of blood testing results across various jurisdictions. Regulatory compliance encompasses numerous practices that validate testing methods, ensure safety, and promote transparency in laboratory operations. In the context of improving blood test accuracy, compliance is essential for fostering public trust and confidence in diagnostic processes.
Regulatory authorities such as the Food and Drug Administration (FDA) and the European Medicines Agency (EMA) establish stringent guidelines for laboratory testing, covering everything from equipment standards to proficiency testing requirements. Laboratories must adhere to these regulations to demonstrate that their testing procedures meet established quality and safety benchmarks. This commitment to compliance not only enhances the accuracy of blood tests but also protects patient health and safety.
Moreover, regulatory compliance facilitates the global exchange of diagnostic information. As healthcare becomes increasingly interconnected, laboratories must ensure their testing practices align with international standards. This alignment fosters collaboration among laboratories and enhances the comparability of test results worldwide, which is invaluable for public health initiatives and research studies.
As the landscape of blood testing continues to evolve, the importance of regulatory compliance will only amplify. Laboratories must remain vigilant in keeping abreast of changing regulations and adapting their practices accordingly. By prioritizing compliance, laboratories can enhance the integrity of their testing processes and contribute to the ongoing advancement of blood test accuracy improvements.
Advanced Data Analysis Techniques to Enhance Blood Test Accuracy
Utilizing Machine Learning Algorithms for Superior Diagnostics
The advent of machine learning has revolutionized healthcare diagnostics, enabling substantial advancements in blood test accuracy improvements. These algorithms possess the capability to analyze vast datasets, uncovering patterns and correlations that may not be immediately apparent to human analysts. This feature is particularly beneficial in blood testing, where the complex interactions among various biomarkers can complicate interpretations.
By training machine learning models on extensive datasets, researchers can develop algorithms that predict disease risks and outcomes based on blood test results. For instance, in the field of oncology, machine learning can assist in recognizing specific biomarkers associated with various cancer types, facilitating personalized treatment strategies. These algorithms enhance blood test accuracy by improving the ability to differentiate between benign and malignant conditions, ultimately leading to improved patient management.
Furthermore, machine learning can streamline diagnostic processes. By automating the analysis of blood test results, healthcare professionals can save valuable time and concentrate more on patient care. This increased efficiency does not compromise accuracy; rather, it complements the overarching goal of delivering dependable diagnostic information promptly.
As machine learning technologies continue to develop, their applications in blood testing are likely to expand. New algorithms and models will emerge, further enhancing blood test accuracy and opening new avenues for research and discovery. The incorporation of machine learning into laboratory practices represents a significant advancement in the quest for improved blood test accuracy.
Applying Statistical Methods for Reliable Blood Test Interpretation
Advanced statistical methods are essential for interpreting blood test results, contributing significantly to improved accuracy. These techniques enable healthcare professionals to evaluate the reliability of test outcomes and make informed clinical decisions. By utilizing statistical methods, clinicians can better understand the significance of test results, minimizing the risk of false positives.
One fundamental statistical method employed in blood testing is the calculation of sensitivity and specificity. Sensitivity assesses a test’s ability to accurately identify true positives, while specificity evaluates its capacity to correctly identify true negatives. By analyzing these parameters, clinicians can determine the reliability of a particular test and its relevance to specific patient populations.
Moreover, statistical methods such as regression analysis facilitate the exploration of relationships between various biomarkers and disease conditions. This exploration enables researchers to identify potential risk factors and develop predictive models that enhance diagnostic accuracy. By leveraging statistical techniques, healthcare professionals can provide more nuanced interpretations of blood test results, ultimately improving patient care.
Additionally, implementing statistical quality control techniques ensures that laboratory processes remain robust and dependable. By routinely monitoring test performance through statistical analyses, laboratories can detect trends and address any deviations from expected results, thereby maintaining high standards of accuracy.
The continuous integration of advanced statistical methods into blood testing practices is vital for enhancing the credibility and reliability of diagnostic information. As these methods evolve, their influence on blood test accuracy improvements will grow increasingly significant, shaping the future of diagnostic medicine.
Leveraging Big Data for Enhanced Blood Test Accuracy
The integration of big data in blood testing is transforming the analysis and interpretation of diagnostic information. The ability to aggregate and examine vast amounts of data from various sources enhances the predictive capacity of blood tests, significantly contributing to improved accuracy. By harnessing big data, healthcare professionals can develop deeper insights into patient health and emerging disease trends.
One of the primary benefits of incorporating big data is the ability to identify patterns and correlations that might otherwise remain hidden. By analyzing extensive datasets from diverse patient populations, researchers can discover new biomarkers associated with specific diseases, leading to more accurate and targeted blood tests. This capability is particularly advantageous in conditions like diabetes and cardiovascular disease, where early detection can have a profound impact on patient outcomes.
Moreover, big data integration facilitates the creation of predictive analytics models that can stratify patients according to their risk profiles. By leveraging machine learning algorithms on large datasets, healthcare providers can identify individuals at heightened risk for developing certain conditions, allowing for proactive interventions. This shift towards predictive medicine aligns seamlessly with the broader trend of personalized healthcare, where treatments are customized to individual patient characteristics.
Additionally, incorporating big data can enhance clinical decision-making. By equipping clinicians with comprehensive insights derived from extensive datasets, healthcare professionals can make more informed choices regarding diagnosis and treatment. This data-driven approach is essential for improving patient outcomes and optimizing healthcare resources.
As big data continues to permeate the field of blood testing, its role in enhancing blood test accuracy improvements will become increasingly prominent. The potential to leverage vast datasets for improved diagnosis and treatment signifies a transformative opportunity for the future of healthcare.
Biomarker Discovery and Its Impact on Enhancing Blood Test Accuracy
Exploring Proteomics for New Biomarkers in Accurate Diagnostics
Proteomics, the in-depth analysis of proteins within biological contexts, serves as a cornerstone of contemporary biomedical research and plays a critical role in identifying new biomarkers for blood tests. By detecting and quantifying proteins associated with various diseases, proteomics significantly enhances blood test accuracy improvements, leading to more precise diagnostics and therapeutic targets.
The extensive data generated from proteomic analysis allows researchers to uncover proteins that may act as early indicators of disease onset or progression. For example, in the realm of cancer, specific protein signatures can be identified in patients’ blood, enabling early diagnosis and ongoing monitoring of treatment effectiveness. This capability to pinpoint disease-specific proteins greatly contributes to the precision of blood tests, ultimately enhancing patient outcomes.
Innovations in proteomic techniques, such as mass spectrometry and protein microarrays, have significantly advanced the analysis of complex protein mixtures with remarkable sensitivity. These technologies enable the simultaneous identification of hundreds of proteins in a single blood sample, offering a comprehensive overview of the proteomic landscape. This high-throughput capability is particularly advantageous for biomarker discovery, allowing the exploration of vast datasets that can yield novel insights into disease mechanisms.
Furthermore, integrating proteomics with other omics technologies, such as genomics and metabolomics, fosters a holistic understanding of disease processes. This systems biology approach enhances the identification of biomarkers that are not only specific but also sensitive to changes in disease status. As proteomics research evolves, its impact on improving blood test accuracy will become increasingly significant, paving the way for innovative diagnostic solutions.
Utilizing Metabolomics for Enhanced Blood Test Insights
Metabolomics, the study of metabolites within biological systems, is gaining prominence for its potential to revolutionize blood testing. By analyzing small molecules produced during metabolic processes, researchers can uncover valuable insights into disease states, significantly contributing to improved blood test accuracy. This approach enables the identification of unique metabolic signatures linked to various conditions, paving the way for innovative diagnostic tools.
The application of metabolomics in blood testing provides a snapshot of an individual’s metabolic health, reflecting changes that may arise due to disease. For instance, fluctuations in metabolite levels can signal the onset of conditions such as diabetes, cardiovascular diseases, and even certain types of cancer. The ability to detect these alterations early enhances blood test accuracy, allowing for timely interventions and improved patient management.
Advancements in analytical techniques, such as nuclear magnetic resonance (NMR) spectroscopy and mass spectrometry, have propelled metabolomics forward. These technologies enable the identification and quantification of a wide array of metabolites in blood samples, allowing researchers to develop comprehensive metabolic profiles. The richness of metabolic data can reveal complex relationships between metabolites and disease pathways, enhancing diagnostic capabilities.
Moreover, combining metabolomics with machine learning algorithms can further boost the predictive power of blood tests. By analyzing intricate metabolic datasets, machine learning models can identify novel biomarkers and patterns, ultimately enhancing diagnostic accuracy. As metabolomics research continues to advance, its role in enhancing blood test accuracy improvements will grow increasingly significant, driving innovations in personalized medicine.
Customizing Blood Testing with Genomic Markers for Enhanced Accuracy
Genomic markers, which reveal insights into an individual’s genetic predispositions, are becoming increasingly crucial in blood testing. The ability to analyze genetic variations carries profound implications for diagnostics and treatment strategies, significantly enhancing improvements in blood test accuracy. By identifying specific genomic markers associated with diseases, clinicians can tailor interventions to individual patients, improving their chances of successful outcomes.
For instance, pinpointing particular gene mutations can guide treatment decisions in cancer diagnostics. Targeted therapies designed to address specific genetic alterations have emerged as powerful tools in oncology. By utilizing genomic markers, healthcare professionals can select therapies more likely to be effective for each patient, optimizing treatment plans and minimizing unnecessary side effects.
Integrating genomic testing into routine blood assessments facilitates earlier identification of genetic predispositions to various conditions. For example, individuals with certain genomic markers may be at elevated risk for developing diseases such as breast cancer or colon cancer. By identifying these markers through blood tests, healthcare providers can implement preventative measures, including increased surveillance and lifestyle modifications, to mitigate risk.
Furthermore, next-generation sequencing technologies have made it feasible to rapidly and affordably analyze an individual’s entire genome. This accessibility has revolutionized the field of genomics, enabling large-scale studies that identify novel genetic markers associated with diseases. As genomic research continues to expand, its impact on enhancing blood test accuracy improvements will be critical, ushering in a new era of personalized medicine.
Strategies for Clinical Validation to Ensure Blood Test Accuracy Enhancements
The Essential Role of Large-Scale Trials in Test Validation
Conducting large-scale clinical trials is vital for validating the reliability and applicability of new blood tests. These trials are crucial for establishing the clinical utility of diagnostic tools and ensuring they provide accurate and meaningful information for patient management. In the pursuit of improving blood test accuracy, rigorous clinical validation is essential for gaining acceptance within the medical community.
Large-scale trials involve evaluating new blood tests across diverse patient populations, allowing researchers to assess their performance across various demographics and disease states. This comprehensive approach guarantees that the tests are accurate in controlled environments and applicable in real-world clinical settings. By studying a wide range of patients, researchers can identify potential limitations and refine the tests as necessary.
Moreover, the results of large-scale trials yield critical evidence for regulatory agencies, facilitating the approval process for new blood tests. Regulatory compliance is essential in ensuring diagnostic tools meet safety and efficacy standards before clinical use. The successful completion of large-scale trials instills confidence in healthcare providers and patients alike, reinforcing trust in the accuracy and reliability of new tests.
In addition to validating test performance, large-scale trials can lead to the discovery of new biomarkers and insights into disease mechanisms. By analyzing patient data collected during these trials, researchers can uncover novel correlations and relationships that may pave the way for developing additional diagnostic tools. As research in this domain progresses, the importance of large-scale trials in enhancing blood test accuracy improvements will remain integral to advancing diagnostic medicine.
Longitudinal Studies: Monitoring Changes Over Time for Accuracy Validation
Longitudinal studies are essential for monitoring changes over time and validating the accuracy of blood tests in assessing disease progression. By observing patients over extended periods, researchers can evaluate how accurately blood tests reflect changes in health status, thereby contributing to improved blood test accuracy. This approach is particularly beneficial for understanding chronic conditions, where biomarker fluctuations are common.
Collecting patient data at multiple time points enables researchers to establish trends and correlations that might not be evident in cross-sectional studies. For instance, in chronic diseases such as diabetes, longitudinal studies can reveal how blood glucose levels fluctuate in response to treatment regimens. By validating the accuracy of blood tests in these contexts, clinicians can make more informed decisions regarding patient management.
Furthermore, longitudinal studies provide invaluable insights into the natural history of diseases, enabling researchers to identify critical time points for intervention. This understanding is essential for devising optimal monitoring strategies and therapeutic approaches tailored to individual patients. As longitudinal studies continue to enhance our understanding of disease processes, their impact on improving blood test accuracy will significantly influence future diagnostic practices.
Additionally, longitudinal studies can reveal potential biomarkers for disease progression and treatment response. By analyzing changes in blood test results over time, researchers can identify markers indicating disease stability or deterioration. This information is crucial for clinicians, allowing timely adjustments to treatment plans based on individual patient responses.
In an evolving healthcare landscape, the significance of longitudinal studies in validating blood tests cannot be overstated. Their contributions to understanding disease dynamics and confirming diagnostic accuracy are vital for delivering high-quality patient care.
Comparative Analysis: Benchmarking New Tests for Enhanced Accuracy
Comparative analysis is fundamental in validating new blood tests, enabling researchers to establish benchmarks against existing methods. This process is essential for demonstrating the accuracy and clinical utility of innovative diagnostic tools, significantly contributing to blood test accuracy improvements. By systematically comparing new tests with established standards, clinicians can ensure that innovations yield reliable results.
The comparative analysis evaluates the sensitivity, specificity, and overall performance of new blood tests against established methodologies. This rigorous assessment helps identify potential limitations or areas for improvement in the new tests. By highlighting the advantages of innovative diagnostic tools, comparative analyses can promote broader acceptance among healthcare professionals and patients.
Moreover, comparative analysis can facilitate the identification of unique features of novel blood tests that may offer enhanced diagnostic capabilities. For instance, a new test may demonstrate superior sensitivity for detecting a specific biomarker compared to an existing assay. This insight can drive the adoption of new tests in clinical practice, ultimately improving patient outcomes through more accurate diagnostics.
In addition to validating performance, comparative analysis can contribute to the ongoing refinement of blood testing methodologies. By continuously assessing new tests against established standards, researchers can identify trends and innovations that inform future developments in diagnostic technology. As the field of blood testing evolves, comparative analysis will remain essential for ensuring that advancements translate into tangible improvements in blood test accuracy.
The unwavering commitment to comparative analysis represents a pivotal aspect of the quest for reliable diagnostics in healthcare. By fostering a culture of rigorous evaluation, researchers and clinicians can collaborate to enhance the accuracy and utility of blood tests, ultimately benefiting patient care.
Ethical and Regulatory Considerations in Enhancing Blood Test Accuracy
Navigating Regulatory Approval Processes for Innovative Diagnostic Tools
Efficiently navigating regulatory approval processes is critical when introducing new blood tests to the market. These processes ensure that diagnostic tools meet stringent safety and efficacy standards before they become accessible for clinical use. Regulatory compliance is essential for instilling confidence among healthcare providers and patients regarding blood test accuracy improvements.
Regulatory bodies, such as the FDA and EMA, establish comprehensive guidelines governing the development and evaluation of diagnostic tests. These guidelines encompass various aspects, including laboratory performance, clinical validity, and post-market surveillance. Adhering to these regulations is vital for demonstrating that new blood tests provide reliable and meaningful information for patient management.
The approval process typically involves conducting rigorous clinical trials that assess the performance of new tests across diverse patient populations. These trials are designed to gather robust evidence regarding test accuracy, sensitivity, and specificity. Successfully completing these trials is crucial for obtaining regulatory clearance, allowing new blood tests to enter the healthcare market.
Moreover, regulatory approval processes enhance patient safety by thoroughly vetting diagnostic tools before use. Regulatory bodies protect patients from potentially harmful or unreliable tests by requiring evidence of safety and efficacy. This commitment to patient safety is fundamental to fostering trust in the healthcare system.
As the landscape of blood testing continues to evolve, the importance of regulatory approval processes will only increase. Laboratories and manufacturers must remain vigilant in adhering to changing regulations and standards. By prioritizing compliance, stakeholders can enhance the credibility and accuracy of blood tests, ultimately contributing to improved patient care.
Safeguarding Data Privacy in Blood Testing Practices
Protecting patient data privacy is a fundamental ethical consideration in blood testing. As diagnostic technologies advance, the collection and use of sensitive personal information must be managed responsibly. In the context of improving blood test accuracy, safeguarding data privacy is crucial for maintaining trust and ethical standards within the healthcare system.
As technology becomes increasingly integrated into blood testing, vast amounts of patient data are routinely collected. This data can encompass test results, demographic information, medical histories, and genetic data. Ensuring the confidentiality and security of this information is paramount to protect patients from potential privacy breaches.
Regulatory frameworks, such as the General Data Protection Regulation (GDPR) in the European Union, establish stringent guidelines for data handling and privacy. These regulations require healthcare providers and laboratories to implement robust safeguards to protect patient information from unauthorized access and misuse. Compliance with these regulations is essential for fostering patient trust and ensuring ethical practices in blood testing.
Furthermore, transparent communication with patients regarding data collection and usage is vital for upholding ethical standards. Patients should be informed about how their data will be used, who will have access to it, and the measures taken to protect their privacy. This transparency empowers patients to make informed decisions regarding their healthcare and fosters a sense of ownership over their personal information.
As blood testing continues to advance, data privacy will remain of utmost importance. Healthcare providers and laboratories must prioritize ethical considerations to maintain patient trust and ensure the ongoing advancement of blood test accuracy improvements.
The Importance of Informed Consent in Blood Testing
Ensuring informed consent is a fundamental ethical consideration in the development and implementation of blood tests. Informed consent involves providing patients with comprehensive information about the nature of the test, its purpose, potential risks, and benefits. This process is essential for respecting patient autonomy and ensuring that individuals can make informed decisions regarding their healthcare.
Informed consent is especially critical when introducing new diagnostic tools aimed at improving blood test accuracy. Patients should be aware of any novel technologies or methodologies employed in testing and how these innovations may impact their diagnosis and treatment. This transparency is vital for fostering trust and confidence within the healthcare system.
Moreover, informed consent processes should encompass discussions about the potential implications of test results. For instance, patients should understand how the outcomes of their blood tests may influence their treatment options and overall health. By providing this information, healthcare providers empower patients to actively participate in their healthcare decisions.
Additionally, the ethical principle of informed consent extends to considerations regarding data privacy and the use of personal information. Patients should be informed about how their data will be utilized, stored, and shared, allowing them to make informed choices regarding their participation in testing.
As the field of blood testing continues to evolve, the commitment to informed consent remains vital. Upholding ethical principles in the development and implementation of blood tests will contribute to enhanced blood test accuracy improvements and foster trust in the healthcare system.
Frequently Asked Questions About Blood Test Accuracy
What does blood test accuracy refer to?
Blood test accuracy indicates the extent to which a test accurately identifies the presence or absence of a specific condition or biomarker, thereby minimizing false positives and false negatives.
How do high-sensitivity assays enhance diagnostic accuracy?
High-sensitivity assays can detect lower levels of biomarkers, enabling earlier disease detection and more precise monitoring, thus significantly improving diagnostic capabilities.
What role do automated systems play in improving blood testing accuracy?
Automated systems decrease human error and increase throughput in blood testing, ensuring consistent and standardized results across laboratories, ultimately enhancing overall accuracy.
How does microfluidic technology contribute to blood test reliability?
Microfluidic technology enables precise control over small sample volumes, allowing simultaneous analysis of multiple biomarkers and improving the reliability of test results.
Why is the use of standardized reference materials significant?
Standardized reference materials ensure the consistency and comparability of test results on a global scale, which is essential for validating blood tests and establishing their credibility.
How does machine learning enhance diagnostic practices?
Machine learning algorithms analyze extensive datasets to identify patterns and improve the accuracy of blood tests, aiding in the early detection of diseases and better patient outcomes.
Why is regulatory compliance critical in blood testing?
Regulatory compliance ensures that blood tests meet safety and efficacy standards, instilling confidence in healthcare providers and patients regarding diagnostic accuracy.
How do longitudinal studies validate blood tests?
Longitudinal studies monitor patient changes over time, validating the accuracy of blood tests in assessing disease progression and informing clinical decisions.
What ethical considerations are involved in data privacy in blood testing?
Data privacy is vital for protecting patient information from breaches, maintaining trust in the healthcare system, and ensuring that ethical standards are upheld in diagnostic practices.
What does informed consent entail in blood testing?
Informed consent involves providing patients with comprehensive information about blood tests, including their purpose, risks, and potential implications, thus enabling informed healthcare decisions.
Connect with us on Facebook!
This Article Was First Found On https://bloodtest.co.uk
The Article: Blood Test Accuracy: Significant Advances Unveiled appeared first on: https://ezbloodtest.com
The Article Blood Test Accuracy: Major Breakthroughs Revealed Was Found On https://limitsofstrategy.com





Comments are closed