Grasping the Vital Role of Temperature Measurement in South Africa’s Healthcare
Understanding the Critical Importance of Accurate Temperature Monitoring for Health
Monitoring body temperature is a fundamental aspect of healthcare in <a href="https://limitsofstrategy.com/goose-valley-golf-club-the-top-golf-course-in-south-africa/">South Africa</a>, where the conditions vary dramatically from coastal warmth to highland chill. Elevated body temperatures can indicate serious health concerns, such as infections, that necessitate prompt medical intervention. Due to South Africa’s diverse population and distinct ecological zones, precise temperature monitoring becomes essential. For instance, in regions with substantial elevation differences like the Drakensberg, individuals may have varying baseline temperatures influenced by their environment. This variability can significantly impact health assessments and subsequent treatment plans. Therefore, acquiring proficiency in accurate temperature measurement and interpretation is vital for effectively managing health across various demographic segments.
Diving Deeper into the Various Temperature Measurement Techniques
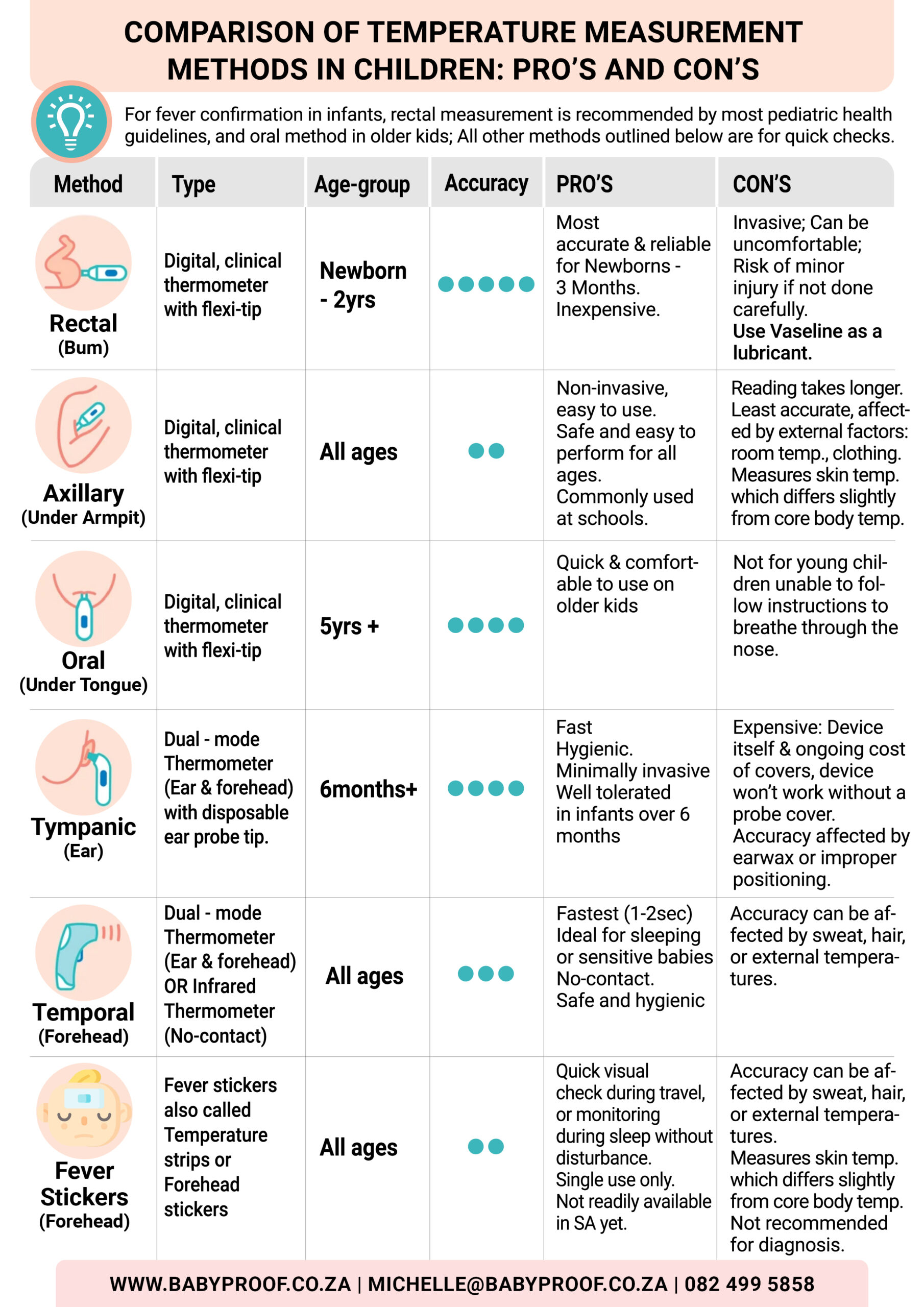
In South Africa, common techniques for measuring body temperature include oral, axillary, and rectal methods, each offering unique benefits and practical considerations tailored to specific contexts. Oral thermometers are widely available in homes and clinics, providing a reliable yet convenient option. While axillary measurements are often utilized in schools and childcare settings due to their non-invasive nature, they are generally regarded as less precise. On the other hand, rectal measurements, although less prevalent outside clinical settings, are considered the gold standard for accuracy, particularly for vulnerable populations such as infants or critically ill patients. Familiarity with these methods and their appropriate applications is crucial for effective health monitoring in South Africa.
Optimizing Temperature Measurement Techniques for Different Age Groups
- Newborn – 3 months → Utilize Rectal (most reliable) or Temporal (forehead) for quick screenings.
- 3 months – 3 years → Rectal for accuracy; Temporal (forehead) or Axillary (underarm) for comfort.
- 4 – 5 years → Oral if the child can cooperate; Temporal (forehead), Tympanic (ear), Axillary (underarm) for quick checks. Fever Stickers can also be considered.
- 6+ years → Oral for the best combination of accuracy and comfort; Temporal (forehead) or Tympanic (ear) for quick assessments.
The Crucial Significance of Accurate Temperature Readings for Health Outcomes
Accurate temperature readings are fundamental in diagnosing illnesses and monitoring health, particularly in a diverse nation like South Africa, where environmental conditions can significantly impact physiological responses. In clinical environments, healthcare professionals depend on precise temperature measurements to make informed treatment decisions. For instance, an inaccurately recorded temperature can lead to unnecessary treatments or delays in critical health interventions. Moreover, during community health initiatives, ensuring accurate temperature readings can enhance the effectiveness of public health responses, especially during infectious disease outbreaks. Thus, the importance of accuracy in temperature measurement is paramount, as it directly influences patient outcomes.
Recognizing the Impact of Altitude on Temperature Measurement Accuracy
The diverse altitudes of South Africa pose unique challenges for temperature measurement. For example, areas like Johannesburg, situated approximately 1,753 meters above sea level, may exhibit different body temperature readings compared to coastal cities like Durban. Increased altitude can alter body metabolism and thermoregulation, requiring careful adjustments when interpreting temperature data. Healthcare providers must consider these variations when evaluating patients from different regions. For instance, a fever in a patient from a high-altitude area may manifest differently than in someone from a lower elevation. Recognizing these nuances is essential for accurate health assessments and personalized patient care.
Embracing Innovations in Temperature Monitoring Technology
Recently, South Africa has experienced substantial technological advancements that improve the efficiency and accuracy of temperature monitoring. Innovations such as infrared thermometers and digital devices are gaining popularity in both clinical and home settings. These devices provide swift readings and often come equipped with user-friendly features, including backlit displays and memory functions. Additionally, smartphone-connected thermometers are emerging, enabling users to track temperature readings over time and share this data effortlessly with healthcare providers. These technological advancements not only streamline the temperature measurement process but also have the potential to enhance health outcomes by facilitating timely medical interventions.
Mastering the Technique of Oral Temperature Measurement in South Africa
A Comprehensive Guide to Accurately Taking an Oral Temperature Reading
Taking an oral temperature reading is a straightforward process that involves placing the thermometer under the tongue while ensuring the mouth remains closed for an accurate measurement. Before taking the reading, it’s essential to confirm that the patient has not consumed any hot or cold food or beverages for at least 15 minutes, as these can interfere with the results. Once the thermometer is positioned, wait for the device to signal that the reading is complete, typically with a beep. Educating patients and caregivers on this technique is vital to ensure it is performed correctly, thereby avoiding inaccurate readings. This method is commonly employed in South African households, making it accessible for family members to conveniently monitor their health.
The Benefits of Utilizing Oral Temperature Measurement Techniques
Oral temperature measurement offers numerous advantages, making it a preferred choice in many South African households and healthcare environments. To begin with, this method is non-invasive, significantly minimizing discomfort often associated with other temperature-taking techniques. It is also user-friendly, allowing individuals to take readings without needing professional assistance. This convenience is particularly beneficial for quick checks at home, enabling families to easily monitor fevers in both children and adults. Furthermore, oral thermometers typically deliver rapid results, usually within one to two minutes, facilitating timely health decisions. In the fast-paced environments of South Africa, this efficiency is especially valuable.
Understanding the Limitations and Considerations of the Oral Method
While oral temperature measurement boasts several advantages, it is not without its limitations. This method may not be suitable for all patient demographics, particularly young children or individuals unable to maintain the thermometer’s position for the required duration. Moreover, factors such as recent food or drink consumption, smoking, or even mouth breathing can compromise the accuracy of readings. In South Africa, where environmental conditions can vary significantly, outdoor temperatures can also affect readings if the thermometer is not used correctly. Therefore, it is essential to consider these factors to achieve the most accurate results possible when utilizing the oral method.
Examining Axillary Temperature Measurement Techniques in South Africa
A Step-by-Step Guide to Properly Measuring Temperature Using the Axillary Method
The axillary method involves placing the thermometer in the armpit and ensuring that the arm is pressed snugly against the body for an accurate reading. This technique is widely adopted in South African schools and childcare facilities due to its safety and ease of execution for individuals of all ages. It is crucial to ensure the skin is dry and that the thermometer is correctly positioned for optimal accuracy. The reading may take longer than oral methods, often requiring several minutes. Educating caregivers and staff on the proper technique is essential to guarantee reliable temperature readings for identifying health issues in both children and adults.
The Advantages of Employing Axillary Temperature Measurement
Axillary temperature measurement offers several benefits, particularly in public health settings throughout South Africa. One of its primary advantages is its non-invasive nature, making it safe for individuals of all ages, including infants and the elderly. The ease of performing this method allows for quick execution in school health programs or health fairs, where time constraints may exist. Additionally, the axillary approach is cost-effective, requiring fewer resources compared to advanced digital or infrared thermometers. This accessibility is especially crucial in rural regions where healthcare resources may be limited. The simplicity and safety of axillary measurements render them an excellent option for community health initiatives.
Identifying Factors That Influence the Accuracy of Axillary Temperature Measurements
Despite its advantages, several factors can affect the accuracy of temperature readings obtained through the axillary method. Environmental conditions, such as high ambient temperatures or humidity prevalent in South Africa, may lead to elevated readings due to perspiration, potentially indicating a false fever. Moreover, clothing can create insulation, hindering heat exchange, which may distort results. Movement during the measurement process, especially in children, can also lead to inaccurate readings. Hence, healthcare providers and caregivers must be aware of these factors and implement strategies to mitigate their impact, such as ensuring the arm remains close to the body and that the skin is dry before taking measurements.
In-Depth Understanding of Rectal Temperature Measurement Techniques in South Africa
A Detailed Approach to Correctly Measuring Rectal Temperature
Accurately measuring rectal temperature involves several steps to ensure both precision and patient comfort. First, it is crucial to apply lubricant to the tip of the thermometer to facilitate gentle insertion. The thermometer should be inserted about an inch into the rectum while being held securely, waiting for the reading to complete. This method is frequently utilized in South African hospitals for its precision, particularly in critical care situations or when monitoring infants. Given its sensitivity, performing the process gently and with the patient’s comfort in mind is essential to maintain trust and cooperation from patients, especially those who are vulnerable.
Understanding Why Rectal Temperature Measurement is Considered the Most Accurate
Rectal temperature measurements yield the most accurate readings in comparison to oral and axillary methods, rendering them ideal for critical care situations in South Africa. This accuracy is especially crucial in emergency contexts or when dealing with unresponsive patients, as healthcare professionals rely on precise temperature data to guide treatment decisions. Additionally, rectal thermometers are less susceptible to external variables, such as ambient temperature or recent oral intake, making them a reliable option in clinical practice. In pediatric care, especially for infants, rectal measurements provide an authoritative assessment of core body temperature, enabling timely and appropriate medical responses.
Key Considerations and Precautions for Using the Rectal Method
Despite its advantages, the rectal measurement method necessitates certain considerations and precautions. The insertion process can be uncomfortable, potentially leading to patient resistance, particularly in non-clinical settings. Therefore, it is vital to clearly explain the procedure and reassure the patient to foster cooperation. Furthermore, healthcare providers must adhere to strict hygiene protocols to prevent any potential infections or injuries. Due to these concerns, rectal measurements are less frequently performed in home settings across South Africa. Nonetheless, understanding when and how to utilize this method is critical for healthcare professionals to ensure the utmost care and accuracy in temperature monitoring.
Expert Insights on Selecting the Most Suitable Temperature Measurement Method
Guidance from South African Health Experts on Temperature Measurement Choices
Health professionals in South Africa frequently recommend various temperature measurement methods based on numerous factors, including the patient’s age, health condition, and specific context. For example, oral measurements are typically advised for adults and older children who can securely hold the thermometer. Conversely, axillary readings might be favored for quick assessments in schools or community health screenings. Rectal measurements are generally recommended for infants or critically ill patients due to their accuracy. Below are some expert recommendations:
- For adults: Prefer oral or rectal readings for enhanced accuracy.
- For young children: Use axillary or rectal methods based on cooperation levels.
- For infants: Rectal measurements are the gold standard for precision.
- In school settings: Axillary readings are often adequate for quick health checks.
- In emergencies: Prioritize rectal measurements for accurate assessments.
These recommendations emphasize the importance of choosing the temperature measurement method that is tailored to the individual needs of each patient and the context in which care is provided.
How Environmental Conditions in South Africa Impact Temperature Readings
Environmental factors in South Africa significantly influence temperature readings, necessitating that healthcare providers consider context while interpreting data. For instance, in coastal areas where humidity levels are high, axillary temperature readings may appear artificially elevated due to excessive sweating, potentially leading to misdiagnosis. Similarly, in colder regions like the Drakensberg, ambient temperatures can cause a drop in readings, prompting healthcare professionals to remain vigilant about local conditions. Experts advocate that practitioners adjust their interpretation of temperature data based on these environmental variables, ensuring accurate assessments. This contextual awareness is crucial for appropriate diagnosis and treatment.
Implementing Best Practices for Temperature Measurement in South Africa
Implementing best practices for temperature measurement is vital in South Africa to ensure accurate and reliable readings. These practices include regularly calibrating thermometers to maintain their precision, as poorly calibrated devices can yield misleading results. Moreover, healthcare providers should understand patient conditions and adapt their temperature measurement techniques accordingly. For example, considering a patient’s hydration status can significantly influence readings. Providers should also educate patients and caregivers about the importance of using proper measurement techniques, including timing when to take readings and understanding factors that may affect temperature. By adhering to these best practices, healthcare professionals can significantly improve the quality of care delivered.
Examining the Influence of Cultural Beliefs on Temperature Measurement Preferences in South Africa
Cultural beliefs significantly shape temperature measurement preferences in South Africa. Various communities may favor specific methods based on traditional practices or comfort levels. For instance, some cultures might prefer non-invasive methods like axillary measurements due to a preference for less intrusive techniques. Acknowledging these cultural nuances is essential for healthcare providers to deliver culturally sensitive care. Engaging with communities to educate them about the benefits and limitations of each temperature measurement method can build trust and improve adherence to recommended practices. Furthermore, respecting cultural beliefs while offering evidence-based recommendations can enhance patient cooperation and health outcomes.
Challenges Faced in Implementing Diverse Temperature Measurement Methods in South African Healthcare Facilities
Implementing temperature measurement methods in South African healthcare facilities presents various challenges, including resource availability and staff training. In rural areas, healthcare facilities may lack access to modern temperature-taking devices, limiting effective monitoring. Additionally, staff may require continuous education and training to ensure they are proficient in accurately using various measurement methods. High patient volumes in urban clinics can also lead to time constraints, resulting in rushed assessments and potential inaccuracies. Addressing these challenges through targeted training programs and improving equipment access is crucial for enhancing temperature monitoring practices throughout South Africa’s diverse healthcare landscape.
Comparative Analysis of Oral, Axillary, and Rectal Temperature Measurement Methods
Identifying the Key Differences Among Temperature Measurement Techniques
The key differences between oral, axillary, and rectal temperature measurement methods primarily revolve around accuracy, ease of use, and suitability for various age groups and settings. Oral thermometers provide dependable readings and are frequently used for adults and older children. However, they require patient cooperation, which may not always be feasible. Axillary temperature measurements are non-invasive and suitable for all ages, making them ideal for community screenings; however, they are generally considered less precise. Rectal measurements, often viewed as the most accurate, may cause discomfort and might not be suitable for all patients outside clinical environments. Understanding these distinctions is essential for selecting the most appropriate method for each situation.
Assessing Accuracy and Reliability Across Various Measurement Methods
In South Africa, the accuracy and reliability of temperature readings differ across the various methods. Rectal measurements are generally recognized as the most accurate, closely reflecting core body temperature. Oral measurements follow, yielding reliable readings when performed correctly, while axillary measurements typically result in the least accurate outcomes. This hierarchy of accuracy guides healthcare providers in their choices, especially when assessing febrile patients or making critical care decisions. For instance, in emergency settings, rectal readings may be prioritized to ensure precise monitoring of patients’ conditions. Acknowledging the limitations of each method can significantly enhance healthcare quality in South Africa.
Evaluating the Suitability of Each Temperature Measurement Method in South African Contexts
The appropriateness of each temperature measurement method within South African contexts depends on various factors, such as the setting and the patient’s specific needs. In home environments, oral measurements are often favored for older children and adults due to their convenience. In contrast, axillary measurements may be standard in schools or during community health campaigns, where quick assessments are necessary. Rectal measurements, while ideal for precise monitoring in clinical settings, may be less suitable for home use due to comfort concerns. Therefore, healthcare providers must carefully evaluate each situation, considering available resources and the patient’s condition to determine the most suitable temperature measurement method.
Practical Considerations for Ensuring Effective Temperature Measurement in South Africa
Exploring the Available Equipment and Resources for Temperature Measurement in South Africa
The range of equipment and resources for temperature measurement in South Africa varies greatly. From basic digital thermometers to advanced clinical devices, the options available are extensive. In urban hospitals, cutting-edge technology is often utilized, including infrared thermometers that allow for rapid and contactless measurements. Conversely, in rural settings, basic thermometers may be the only option, which can affect the accuracy of readings. The availability and affordability of these tools greatly influence healthcare practitioners’ choice of methods across the country. Ensuring that healthcare facilities, particularly in underserved areas, have access to reliable equipment is crucial for effective patient care.
Challenges Encountered in Temperature Measurement Practices
Healthcare providers in South Africa face numerous challenges regarding temperature measurement. Limited resources, especially in rural regions, can restrict access to accurate and reliable thermometers. Furthermore, patient cooperation can be unpredictable, particularly in children or individuals with cognitive impairments, making accurate measurement difficult. Unique environmental factors, such as extreme heat or cold, can also interfere with readings and complicate assessments. Overcoming these challenges involves employing strategies such as community education initiatives, improving equipment access, and training healthcare providers on best practices for temperature measurement.
Strategies for Achieving Accurate Temperature Readings in South Africa
Achieving accurate temperature readings in South Africa involves several critical steps. First, healthcare providers should consistently evaluate their techniques to ensure adherence to best practices for each measurement method. Regular calibration of thermometers is also essential to maintain accuracy. Educating patients and caregivers about the significance of proper technique, including factors that can influence readings, such as recent food intake or environmental temperature, can greatly enhance assessment reliability. Practitioners should also consider the distinct environmental conditions of South Africa to appropriately adjust their interpretation of readings, thereby ensuring comprehensive patient care.
Proven Strategies for Selecting the Best Temperature Measurement Method
Guidelines for South Africans to Choose the Most Effective Measurement Technique
Selecting the best method for temperature measurement in South Africa necessitates careful consideration of several factors. First, the patient’s age and health condition significantly influence the appropriate method. For example, infants may necessitate rectal measurements for accuracy, while older children might be more suited to oral or axillary methods. Additionally, the setting—whether in a clinical environment, at home, or during a community health event—should guide the choice of measurement. South Africans can adopt these strategies to ensure informed decision-making:
- Assess the patient’s age and level of cooperation.
- Consider the urgency of the temperature assessment.
- Evaluate available equipment and resources.
- Be aware of environmental conditions that may affect readings.
By following these steps, individuals can ensure they select a method that delivers reliable results.
Best Practices for Each Temperature Measurement Method in South Africa
Implementing best practices for temperature measurement is critical across all methods used in South Africa. For oral measurements, always confirm that the patient has not consumed anything that could affect readings beforehand. When performing axillary measurements, keeping the arm close to the body and ensuring the skin is dry will yield more accurate results. Rectal measurements require careful handling and clear communication with the patient to minimize discomfort. Best practices for each method include:
- Regularly calibrate thermometers to ensure accurate readings.
- Educate patients and caregivers on proper techniques.
- Consider environmental factors when interpreting results.
- Document findings accurately to facilitate ongoing health assessments.
Following these practices will enhance the reliability of temperature measurements and improve health outcomes throughout South Africa.
Strategies for Educating the South African Public on Temperature Measurement Practices
Public education on temperature measurement is essential for enhancing health literacy across South Africa. Healthcare providers can establish clear guidelines that outline the importance of accurate temperature readings and how to measure them effectively. Community outreach programs, workshops, and health fairs can serve as platforms to educate the public about various temperature measurement methods. Moreover, utilizing local healthcare resources, such as clinics and hospitals, to disseminate information and provide demonstrations can improve understanding. By focusing on practical application and cultural relevance, healthcare professionals can foster a more informed public capable of effectively monitoring their health.
Assessing the Most Effective Temperature Measurement Method in South Africa
Key Insights on Temperature Measurement Practices
Oral, axillary, and rectal temperature measurement methods each possess distinct advantages and limitations within South African healthcare. Understanding the unique characteristics of each method, including accuracy, ease of use, and age appropriateness, is crucial for effective health monitoring. By being aware of the environmental factors that can influence readings, healthcare professionals can make informed decisions that enhance patient care.
Guidelines for Healthcare Providers in South Africa
Healthcare providers in South Africa should consider individual patient needs, including age and health status, when selecting temperature measurement methods. Furthermore, they should remain cognizant of available resources and the environmental context to ensure accurate assessments. Ongoing training and education on the latest best practices will further empower providers to deliver high-quality care in temperature monitoring.
Emerging Trends in Temperature Measurement Technology in South Africa
Future trends in temperature measurement may include the adoption of advanced technologies, such as smart thermometers that connect to mobile applications for tracking health metrics. Enhanced public education initiatives can further elevate health literacy regarding temperature measurement. Additionally, tailored approaches that consider South Africa’s unique cultural and environmental contexts will improve the effectiveness of healthcare delivery in temperature monitoring.
Addressing Disparities Between Rural and Urban Temperature Measurement Practices
The choice of temperature measurement methods may differ dramatically between rural and urban settings in South Africa. Limited access to advanced equipment in rural areas may necessitate reliance on simpler methods like axillary readings. In contrast, urban facilities often have access to a wider array of technological options, permitting more precise measurements. Addressing these disparities through targeted resource allocation and training is vital to ensure equitable healthcare access.
The Role of Cultural Practices in Shaping Temperature Measurement Preferences
Cultural beliefs and practices significantly influence attitudes toward temperature measurement methods in South Africa. Understanding and respecting these beliefs is imperative for healthcare providers to deliver culturally sensitive care. By engaging with community leaders and incorporating culturally relevant practices into health education, providers can ensure that temperature measurement methods are accepted and effectively utilized within various cultural contexts.
Frequently Asked Questions About Temperature Measurement Techniques
What is the most accurate method for measuring body temperature?
The rectal method is widely regarded as the most accurate for measuring body temperature, as it closely reflects core body temperature and is less influenced by external factors.
Can axillary temperature be relied upon for accurate diagnosis?
While axillary temperature is non-invasive and safe, it is generally less accurate than oral or rectal methods. However, it can still provide useful information in non-critical settings.
How can I properly take an oral temperature reading?
To take an oral temperature, place the thermometer under the tongue, close the mouth, and wait for it to beep. Ensure that no hot or cold food or drink has been consumed beforehand.
What factors can affect the accuracy of axillary temperature readings?
Factors such as ambient temperature, humidity, clothing, perspiration, and movement can all influence the accuracy of axillary temperature readings.
Is it safe to measure rectal temperature at home?
While rectal measurements are accurate, they can be uncomfortable. They are generally recommended for infants or in clinical settings rather than at home unless advised by a healthcare professional.
What technology is available for temperature measurement in South Africa?
In South Africa, a variety of technologies is available, ranging from basic digital thermometers to advanced infrared devices that enable quick, non-contact temperature measurements.
How often should thermometers be calibrated?
Thermometers should be calibrated regularly to ensure accuracy, ideally before significant use each season or at least once a year.
What should I do if my temperature reading is abnormal?
If a temperature reading is abnormal, especially if accompanied by other symptoms, it is advisable to seek medical advice for further evaluation and potential treatment.
Are there cultural preferences for temperature measurement methods in South Africa?
Yes, cultural beliefs can impact preferences for specific temperature measurement methods. Understanding these beliefs is vital for providing culturally sensitive healthcare.
How can I learn more about temperature measurement techniques?
You can learn more about temperature measurement techniques through local healthcare providers, community health workshops, and online resources dedicated to health education.
Check out our vibes on Instagram!
The article Best Method for Temperature: Oral, Axillary, or Rectal? A South African Guide was published first on: https://www.babyproof.co.za
The Article Temperature Measurement Methods: Oral, Axillary, or Rectal? Was Found On https://limitsofstrategy.com





No responses yet